PARKINSON'S DISEASE

Diagnosis
Currently, there isn't a specific test to diagnose Parkinson's disease. A diagnosis is made by a doctor trained in nervous system conditions, known as a neurologist. A diagnosis of Parkinson's is based on your medical history, a review of your symptoms, and a neurological and physical exam.
A member of your health care team may suggest a specific single-photon emission computerized tomography (SPECT) scan called a dopamine transporter (DAT) scan. Although this can help support the suspicion that you have Parkinson's disease, it is your symptoms and results of a neurological exam that ultimately determine the correct diagnosis. Most people do not require a DAT scan.
Your care team may order lab tests, such as blood tests, to rule out other conditions that may be causing your symptoms.
Imaging tests — such as an MRI, ultrasound of the brain and PET scans — also may be used to help rule out other disorders. Imaging tests aren't particularly helpful for diagnosing Parkinson's disease.
In addition to examining you, a member of your health care team may give you carbidopa-levodopa (Rytary, Sinemet, others), a Parkinson's disease medicine. You must be given a sufficient dose to show the benefit, as getting low doses for a day or two isn't reliable. Significant improvement with this medicine will often confirm your diagnosis of Parkinson's disease.
Sometimes it takes time to diagnose Parkinson's disease. Health care professionals may recommend regular follow-up appointments with neurologists trained in movement disorders to evaluate your condition and symptoms over time and diagnose Parkinson's disease.
However, a new test may be on the horizon. Researchers are studying a Parkinson's test that can detect the disease before symptoms begin. The test is called an alpha-synuclein seed amplification assay. In a 2023 study, researchers tested the spinal fluid of more than 1,000 people to look for clumps of the protein alpha-synuclein. Alpha-synuclein is found in Lewy bodies. It forms clumps that the body can't break down. The clumps spread and damage brain cells.
Alpha-synuclein clumps are a hallmark sign of Parkinson's disease. The test accurately identified people with Parkinson's disease 87.7% of the time. The test also was highly sensitive for detecting people at risk of Parkinson's disease.
This study of the alpha-synuclein seed amplification assay was the largest so far. Some researchers say the study may be a game changer for Parkinson's disease diagnosis, research and treatment trials. But larger studies are needed. There's hope among researchers that in the future, the test could be done using blood samples rather than spinal fluid.
Treatment
Parkinson's disease can't be cured, but medicines can help control the symptoms, often dramatically. In some more advanced cases, surgery may be advised.
Your health care team also may recommend lifestyle changes, especially ongoing aerobic exercise. In some cases, physical therapy that focuses on balance and stretching is important. A speech-language pathologist may help improve speech problems.
Medications
Medicines may help you manage problems with walking, movement and tremor. These medicines increase or substitute for dopamine.
People with Parkinson's disease have low levels of brain dopamine. However, dopamine can't be given directly because it can't enter the brain.
You may have significant improvement of your symptoms after beginning Parkinson's disease treatment. Over time, however, the benefits of medicines frequently diminish or become less consistent. You can usually still control your symptoms well.
Medicines your care team may prescribe include:
Carbidopa-levodopa (Rytary, Sinemet, Duopa, others). Levodopa, the most effective Parkinson's disease medicine, is a natural chemical that passes into the brain and is converted to dopamine.Levodopa is combined with carbidopa (Lodosyn), which protects levodopa from early conversion to dopamine outside the brain. This prevents or lessens side effects such as nausea.Side effects may include nausea or lightheadedness when you stand, called orthostatic hypotension.After years, as your disease progresses, the benefit from levodopa may lessen, with a tendency to wax and wane, also called "wearing off."Also, you may experience involuntary movements known as dyskinesia after taking higher doses of levodopa. Your care team may lessen your dose or adjust the times of your doses to control these effects.Unless told otherwise by your health care team, carbidopa-levodopa is best taken on an empty stomach if you have advanced Parkinson's disease.
Inhaled carbidopa-levodopa. Inbrija is a brand-name medicine delivering carbidopa-levodopa in an inhaled form. It may be helpful in managing symptoms that arise when medicines taken by mouth suddenly stop working during the day.
Carbidopa-levodopa infusion. Duopa is a brand-name medicine combining carbidopa and levodopa. However, it's administered through a feeding tube that delivers the medicine in a gel form directly to the small intestine.Duopa is for patients with more-advanced Parkinson's who still respond to carbidopa-levodopa but who have a lot of fluctuations in their response. Because Duopa is continually infused, blood levels of the two medicines remain constant.Placement of the tube requires a small surgical procedure. Risks associated with having the tube include the tube falling out or infections at the infusion site.
Dopamine agonists. Unlike levodopa, dopamine agonists don't change into dopamine. Instead, they mimic dopamine effects in the brain.Dopamine agonists aren't as effective as levodopa in treating symptoms. However, they last longer and may be used with levodopa to smooth the sometimes off-and-on effect of levodopa.Dopamine agonists include pramipexole (Mirapex ER) and rotigotine (Neupro), which is given as a patch. Apomorphine (Apokyn) is a short-acting dopamine agonist shot used for quick relief.Some of the side effects of dopamine agonists are like the side effects of carbidopa-levodopa. But they also can include hallucinations, sleepiness and compulsive behaviors such as hypersexuality, gambling and eating. If you're taking these medicines and you behave in a way that's out of character for you, talk to your health care team.
Monoamine oxidase B (MAO B) inhibitors. These medicines include selegiline (Zelapar), rasagiline (Azilect) and safinamide (Xadago). They help prevent the breakdown of brain dopamine by inhibiting the brain enzyme monoamine oxidase B (MAO B). This enzyme breaks down brain dopamine. Selegiline given with levodopa may help prevent wearing off.Side effects of MAO B inhibitors may include headaches, nausea or insomnia. When added to carbidopa-levodopa, these medicines increase the risk of hallucinations.These medicines are not often used in combination with most antidepressants or certain pain medicines due to potentially serious but rare reactions. Check with your health care team before taking any additional medicines with an MAO B inhibitor.
Catechol O-methyltransferase (COMT) inhibitors. Entacapone (Comtan) and opicapone (Ongentys) are the primary medicines from this class. This medicine mildly prolongs the effect of levodopa therapy by blocking an enzyme that breaks down dopamine.Side effects, including an increased risk of involuntary movements called dyskinesia, mainly result from an enhanced levodopa effect. Other side effects include diarrhea, nausea or vomiting.Tolcapone (Tasmar) is another COMT inhibitor that is rarely prescribed due to a risk of serious liver damage and liver failure.
Anticholinergics. These medicines were used for many years to help control the tremor associated with Parkinson's disease. Several anticholinergic medicines are available, including benztropine (Cogentin) or trihexyphenidyl.However, their modest benefits are often offset by side effects such as impaired memory, confusion, hallucinations, constipation, dry mouth and impaired urination.
Amantadine. Health care professionals may prescribe amantadine (Gocovri) alone to provide short-term relief of symptoms of mild, early-stage Parkinson's disease. It also may be given with carbidopa-levodopa therapy during the later stages of Parkinson's disease to control involuntary movements called dyskinesia induced by carbidopa-levodopa.Side effects may include a change in skin color, ankle swelling or hallucinations.
Adenosine receptor antagonists (A2A receptor antagonists). These drugs target areas in the brain that regulate the response to dopamine and allow more dopamine to be released. Istradefylline (Nourianz) is one of the A2A antagonist drugs.
Nuplazid (Pimavanserin). This drug is used to treat hallucinations and delusions that can occur with Parkinson's disease. Experts aren't sure how it works.
Surgical procedures
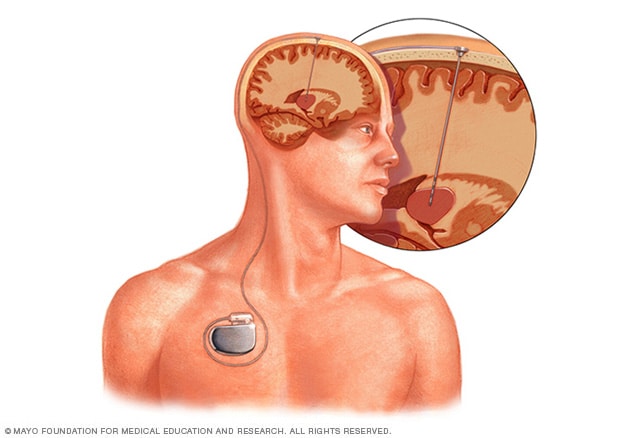
Deep brain stimulation
Deep brain stimulation. In deep brain stimulation (DBS), surgeons implant electrodes into a specific part of the brain. The electrodes are connected to a generator implanted in the chest near the collarbone. The generator sends electrical pulses to the brain and may reduce Parkinson's disease symptoms.Your health care team may adjust your settings as necessary to treat your condition. Surgery involves risks, including infections, stroke or brain hemorrhage. Some people experience problems with the DBS system or have complications due to stimulation. A member of your health care team may need to adjust or replace some parts of the system.Deep brain stimulation is most often offered to people with advanced Parkinson's disease who have unstable responses to levodopa. DBS can stabilize medicine fluctuations, reduce or halt involuntary movements called dyskinesia, reduce tremor, reduce rigidity, and improve movements.DBS is effective for controlling changing responses to levodopa or for controlling dyskinesia that doesn't improve with medicine adjustments.However, DBS isn't helpful for problems that don't respond to levodopa therapy apart from tremor. Tremor may be controlled by DBS even if the tremor isn't very responsive to levodopa.Although DBS may provide sustained benefit for Parkinson's symptoms, it doesn't keep Parkinson's disease from progressing.
